
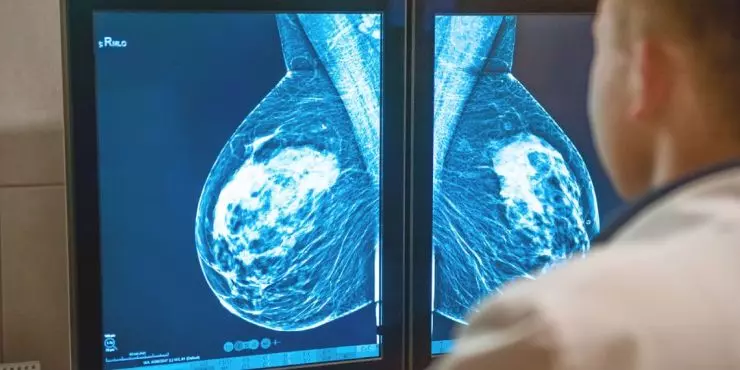
Mammograms can feel a little mysterious until you’ve had one. The short version: a mammogram is a low-dose X-ray of the breast that looks for early signs of breast cancer—often years before a lump can be felt. Early detection matters because it leads to more treatment options and better outcomes.
At Northwest Family Clinics, we help you decide when to start screening, where to go, and how to make the experience as comfortable as possible. Here’s what to know before you book.
When Should I Start Screening?
Most average-risk women begin routine screening at age 40. The exact schedule—every year or every 1–2 years—depends on your personal and family history, prior imaging, and your preferences. If you have a higher risk due to genetics, a strong family history, or prior chest radiation, you may need to start earlier or add breast MRI. Your clinician will help tailor a plan that fits you.
Types of Mammograms
-
Digital mammogram (2D).
Standard, widely available screening and diagnostic imaging. -
Digital breast tomosynthesis (3D mammogram).
Takes multiple images from different angles that a computer reconstructs into thin “slices,” which can improve cancer detection and reduce callbacks, especially in dense breasts. -
Diagnostic mammogram.
Extra views done after a screening callback or to evaluate a specific symptom like a new lump, nipple discharge, or focal pain. Ultrasound may be added the same day.
How to Prepare for a Mammogram
- Schedule when breasts are least tender. For many, that’s the week after your period.
- Bring prior images. If you had mammograms at another facility, ask them to send images ahead of time.
- Skip lotions, deodorant, and powders on the chest and underarms the day of your exam; some products can show up as artifacts.
- Wear a two-piece outfit so you only remove your top and bra.
- Tell the technologist if you’re pregnant, breastfeeding, have implants, or have any new symptoms.
What Happens During the Exam

You’ll change into a gown and stand at the machine. A technologist positions your breast on a flat plate and lowers a top plate to gently but firmly compress the tissue for a few seconds. Compression spreads the tissue so the X-ray can see through it clearly and uses less radiation. Most screening exams include at least two views per breast; 3D adds a short sweep while you hold still. The whole visit typically takes 15–20 minutes, with only seconds of compression per image.
Does it Hurt?
Most people describe brief pressure or discomfort. Communication helps—tell the technologist if you’re tender so they can adjust positioning, use slower compression, or pause between images. Deep, slow breathing and focusing your gaze can reduce muscle tension and make it easier.
What About Radiation?
Mammograms use a low dose of radiation, roughly similar to a few months of natural background exposure. For most women, the benefit of early cancer detection outweighs the small risk from imaging.
Results and Callbacks
Your images are read by a radiologist. Reports are summarized with a BI-RADS assessment, which guides next steps:
- 0: Incomplete—more images or ultrasound needed
- 1–2: Negative/benign—routine screening schedule
- 3: Probably benign—short-term follow-up imaging
- 4–5: Suspicious—talk about biopsy options
A callback does not mean cancer; it means the radiologist wants a closer look. Many callbacks are resolved with extra views or ultrasound and return to routine screening.
Mammograms and Breast Density
Dense breast tissue is common and can make mammograms harder to interpret. If your report mentions density, your clinician may discuss 3D mammography and whether supplemental screening (such as ultrasound or MRI based on risk) makes sense for you.
If You Have Implants
You can and should get mammograms with implants. The technologist will take implant-displaced views to visualize more breast tissue. Be sure to mention implants when scheduling and at check-in.
Minnesota Scheduling and Access
We coordinate screening at trusted imaging centers near our Northwest Family Clinics locations in Crystal, Plymouth, and Rogers. Need help transferring prior images or choosing 2D vs. 3D? Call us—our team will handle the logistics and get you on the books.
FAQs
Do I need a referral?
Many centers allow self-scheduled screening mammograms, but a referral helps ensure results flow back to your clinician. We can place the order and coordinate everything.
How often should I get a mammogram?
Most average-risk women screen every year or every 1–2 years starting at 40. We’ll personalize this based on your history and comfort level.
What if I feel a new lump?
Call us to schedule an appointment or book online. You’ll likely need a diagnostic mammogram and a same-day ultrasound rather than a screening exam.
Can I be screened while breastfeeding?
Yes. Try to feed or pump just before the exam to reduce tenderness. If milk interferes with the images, additional views may be taken.
Is 3D mammography better?
3D can improve detection and reduce callbacks, especially in dense breasts. Availability and insurance coverage vary; we’ll help you decide.
Will insurance cover it?
Screening mammograms are covered by most plans. Diagnostic imaging may have copays or deductibles. Our staff can help you check benefits.
Ready to Schedule?
Whether you’re booking your first mammogram or you’re due for your yearly screening, we’re here to make it straightforward. Contact Northwest Family Clinics in Crystal, Plymouth, or Rogers to set up your appointment and get a screening plan that fits your life.